Last year was a big year for North Carolina. After a decade of action and advocacy, as of this past December, Medicaid Expansion is finally in effect. This is no small accomplishment, even though it is just one step on the road toward truly healthy and equitable communities. Looking ahead, this policy victory will continue to play a major role as those of us at FHLI continue to act, change systems, and improve health.
2023 was also a big year for FHLI. As we kick off the new year, we’re reflecting on everything we were able to accomplish alongside partner organizations and communities across our state. Read on for highlights from 2023 and look forward to what we have planned for 2024.
Roadmap to Innovation
This year FHLI took an important step to innovate our portfolio as an organization. We announced FHLI’s Roadmap to Innovation, which will help communities develop and implement their own paths to health equity. This line of work was built out of our Community Voice model, centering local, participatory decision-making to identify and act on community-driven solutions to health disparities and inequities.
We are leveraging a $900,000 investment in ourselves to work deeply in three groups of contiguous counties across North Carolina to provide support and address social drivers of health. Stay tuned in 2024 as we begin the work to:
- Facilitate community-driven identification of structural issues and systems change advocacy to impact those issues.
- Increase community-based organization access to larger state, federal, and NGO sources of grant dollars.
- Increase efficiency and integration of existing services through community-driven care networks that include traditional and non-traditional partners.
- Increase overall community-based organization capacity to deliver services.
Bertie County Integrated Behavioral Health Network
Throughout this year, FHLI’s Community Voice and Center of Excellence for Integrated Care (COE) teams facilitated a network of local leaders in Bertie County to address their community’s behavioral health needs. The Network leverages FHLI’s Community Voice model, centering participatory engagement to allow communities themselves to identify needs and efficiently drive decision-making around desired outcomes, resource needs, and local and system-wide solutions.
End-of-year update: The Bertie County Integrated Behavioral Health Network received a $300,000 grant from Merck to continue their work in 2024!
Read more
Bringing National Rural Health Day to Rural North Carolina
In 2023, the National Rural Health Association co-hosted a National Rural Health Day celebration with the North Carolina Office of Rural Health (NC ORH). It was an extra special year for two reasons. First, 2023 also marked the NC ORH’s 50th anniversary. Founded by our nonprofit’s founding director, Jim Bernstein, the NC ORH is the oldest office of rural health in the country.
The second reason this year’s celebration was special is because we brought the festivities to rural North Carolinians. Rather than having an event in Raleigh, we hosted the festivities at the Bertie County Aging Council – Senior Center, where the Bertie County Integrated Behavioral Health Network has met throughout the year. Local community members joined state officials and several federal government officials for the day-long event.
Read more
Adding Maternal Health to the FHLI Portfolio
Last year we launched the Maternal and Child Health Equity Action Network (MCHEAN) following our comprehensive landscape report, “Progress and Opportunities: Maternal and Child Health Equity in North Carolina.”
Through this work, we can collaborate with mothers, birthing professionals, and advocates to map out a better future for maternal and child health. This area deserves special focus in North Carolina. According to the latest March of Dimes report card, we are among the worst states in the country for preterm births, with significant racial and economic disparities across the state. This issue is at the forefront of our minds, and we have incorporated a maternal and child health focus into our work in Bertie County and our Roadmap to Innovation, one of FHLI’s newest programs.
Read more
Medicaid Expansion
Medicaid Expansion in North Carolina is a hard-won victory for public health, health care professionals, and everyone in our state. Advocates have been working to make this a reality since 2010 when the Affordable Care Act was passed.
Expansion finally took effect statewide on December 1st, 2023, and is expected to provide over 600,000 people in the health care coverage gap, including veterans, frontline workers, small business owners, parents, and many more, with access to health insurance. This includes residents with incomes too high to qualify for Medicaid but too low to receive health care subsidies through the Affordable Care Act marketplace.
Read more
This comprehensive health coverage includes dental, behavioral health, and vision care.
All of us at FHLI are thrilled to see this important step forward for North Carolina take effect, but we will also continue working hard to improve health access and equity for all North Carolinians.
Specifically, we are focusing our energy on steps to move North Carolina closer toward truly healthy communities. In the new year, we will be developing a 2025-2026 policy advocacy agenda, among other efforts to improve access and equity in care for all North Carolinians.
Read more
National Rural Health Association (NRHA) Rural Health Policy Institute
Early in 2023, we brought our collective voice to Capitol Hill, joining the NRHA for its 34th annual Rural Health Policy Institute.
The Rural Health Policy Institute is an opportunity for rural health leaders across the country to bring community stories to Capitol Hill, guiding the future of rural health policy with NRHA leadership and advocating for important issues with new and returning members of Congress and the presidential administration.
Read more
2023 Legislative Breakfast
Last April, the North Carolina Rural Health Association (NCRHA) and North Carolina Oral Health Collaborative (NCOHC) co-hosted this year’s legislative breakfast. At the event, we presented health care leadership awards to Representative Donna McDowell White (NC House District 26), Senator Jim Burgin (NC Senate District 12), Senator Jim Perry (NC Senate District 2), Dr. Amanda Stroud (Dental Director, AppHealthCare), and Michelle Fortune (CEO, St. Luke’s Hospital).
Read more
During the event, Fortune and Stroud both shared deeply personal stories about their experiences with health and health care in North Carolina.
When Fortune’s father began experiencing chest pain, he was taken to St. Luke’s, his daughter’s hospital. He was cleared and almost sent home before a doctor took time, paid attention, and discovered he was having a heart attack.
St. Luke’s didn’t have a cardiologist at the time. The only solution to a condition that kills nearly 19,000 North Carolinians each year was to load Fortune’s father into a helicopter and fly him to a different hospital equipped to treat heart disease.
St. Luke’s has a cardiologist now, thanks to a sustained increase in funding. Fortune and her father’s story is all too common for people across North Carolina, however, and too many rural hospitals struggle and are unable to provide vital life-saving services.
Stroud also spoke to attendees about her motivation to work as a public health dentist in rural North Carolina.
Stroud grew up on food stamps, with parents who worked long hours in grueling jobs to make ends meet. She didn’t see her first dentist until a school-based program came to her school. Today, she provides that same school-based care to children in Ashe, Alleghany, and Watauga Counties.
Stroud choked up as she talked about the safety net, how it saved her life, and how hard it can be to continue her life-saving work faced with limited funding and staffing shortages.
“Where I’m from, dentures are the norm,” said Stroud. “We need to make dentists the norm.”
Read more
All Aboard the Momnibus!
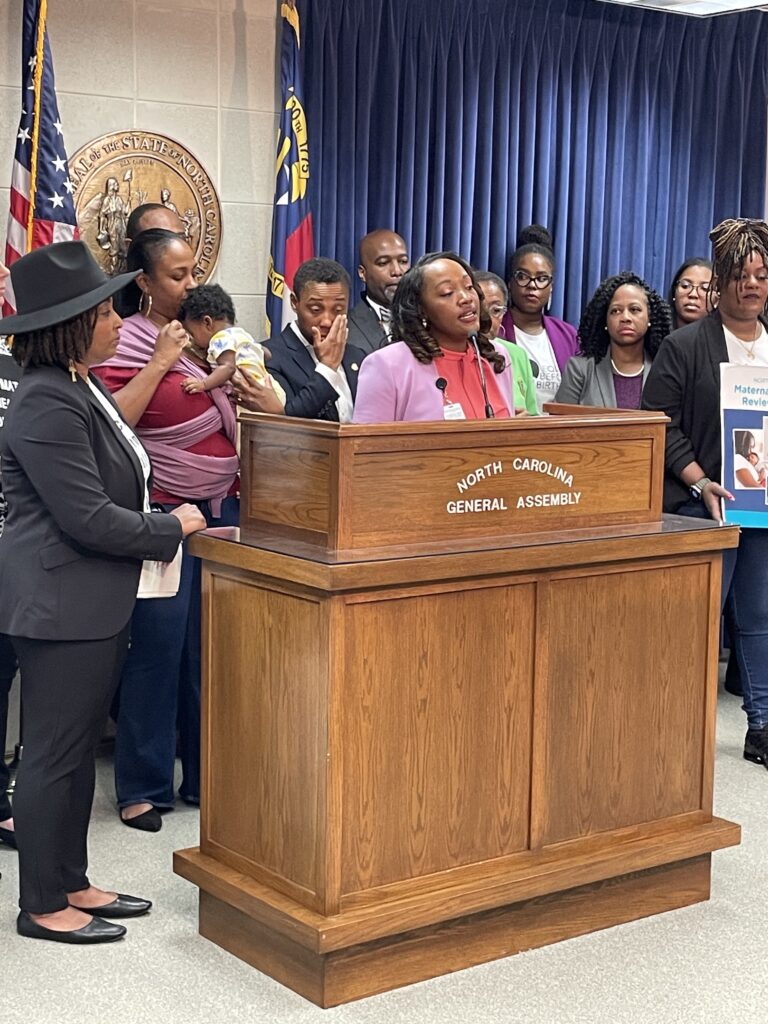
The signs said it all. “Black Maternal Health is Nonpartisan.”
This was the message advocates, providers, and parents took to the legislature for Black Maternal Health Day of Action on April 19, 2023.
We joined advocates, mothers, and providers from across the state to meet with elected officials and discuss the importance of policy action to reduce racial disparities in maternal health across North Carolina.
Read more
Thought leadership: 2023 Rural Health Snapshot and Maternal Health Landscape Report
In 2023 we published another annual edition of the North Carolina Rural Health Association’s (NCRHA) Rural Health Snapshot. FHLI staff unveiled the 2023 report at our legislative breakfast and distributed copies to legislators working to improve rural health in our state.
Our other report published in 2023, a Maternal and Child Health Equity landscape report, earned a prominent feature at the 2023 Black Maternal Health Day of Action at the North Carolina General Assembly.
The Project ECHO Network in North Carolina (PEN-NC)
Early in 2023, we launched a new program in partnership with the North Carolina Area Health Education Centers (NC AHEC). Leveraging NC AHEC’s technical assistance expertise alongside FHLI’s legacy of incubating innovative programs, PEN-NC will serve as the first statewide network of ECHO™ projects.
The ECHO™ Model, originally developed out of the University of New Mexico, is a framework for virtual learning communities where peers can share support, guidance, and feedback.
Read more
Oral Health Day 2023
Bright spots, pressing issues, and goals moving forward for oral health in North Carolina were on full display during Oral Health Day last June. The theme for this year’s event was, “Challenges and Opportunities for the Dental Team.” Keynote speaker Kathy Colville and the other panelists brought expertise and ideas for how North Carolina can become a healthier, more equitable state.
Read more
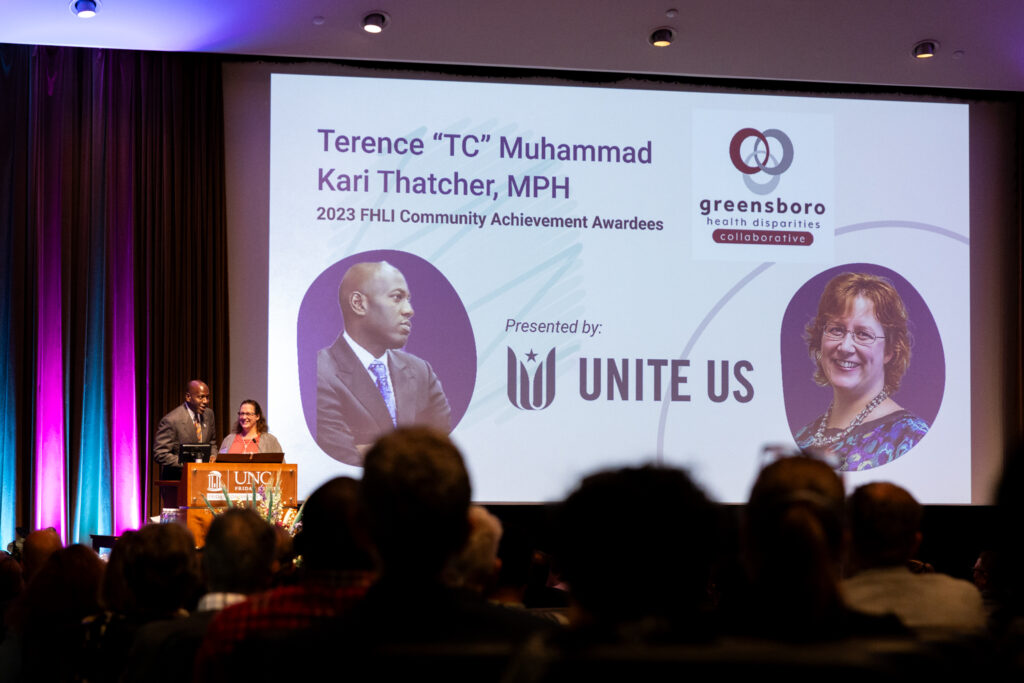
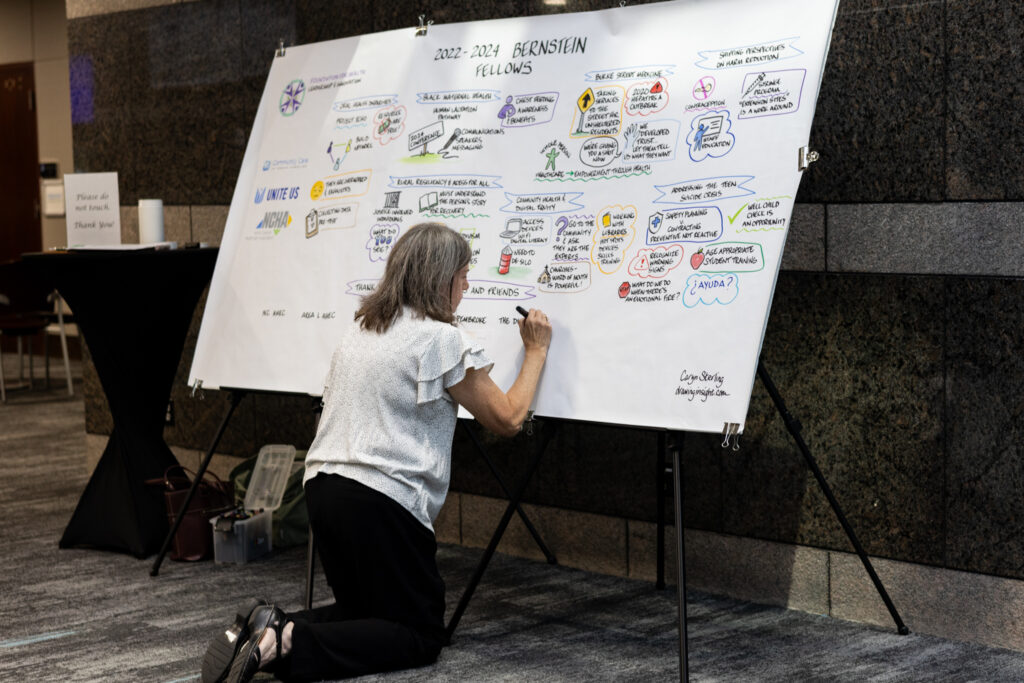
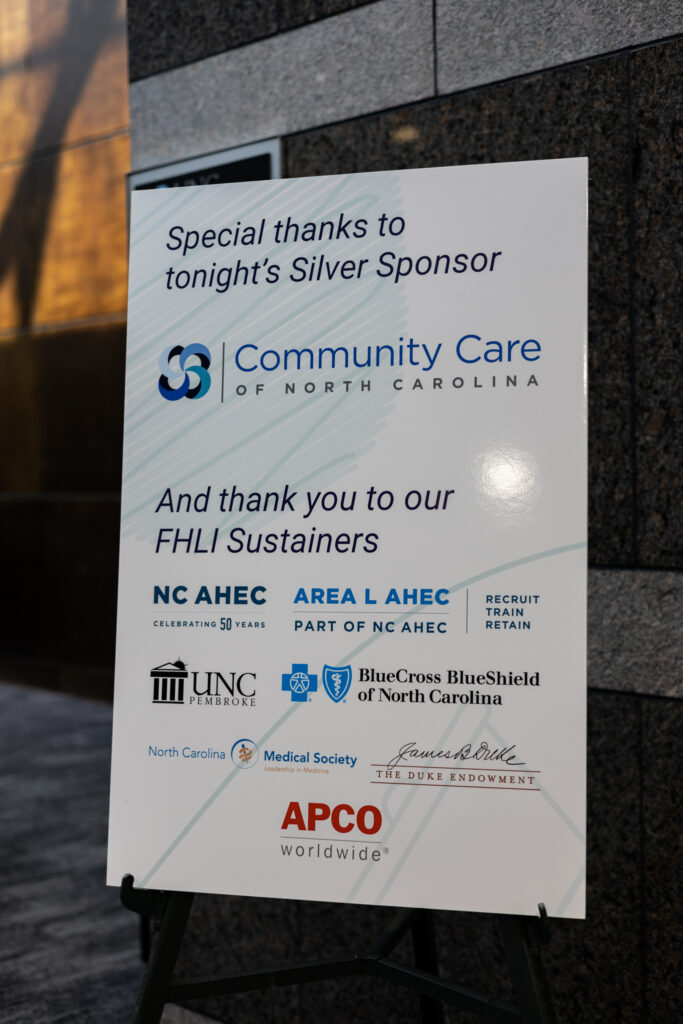
The 2023 Bernstein Event
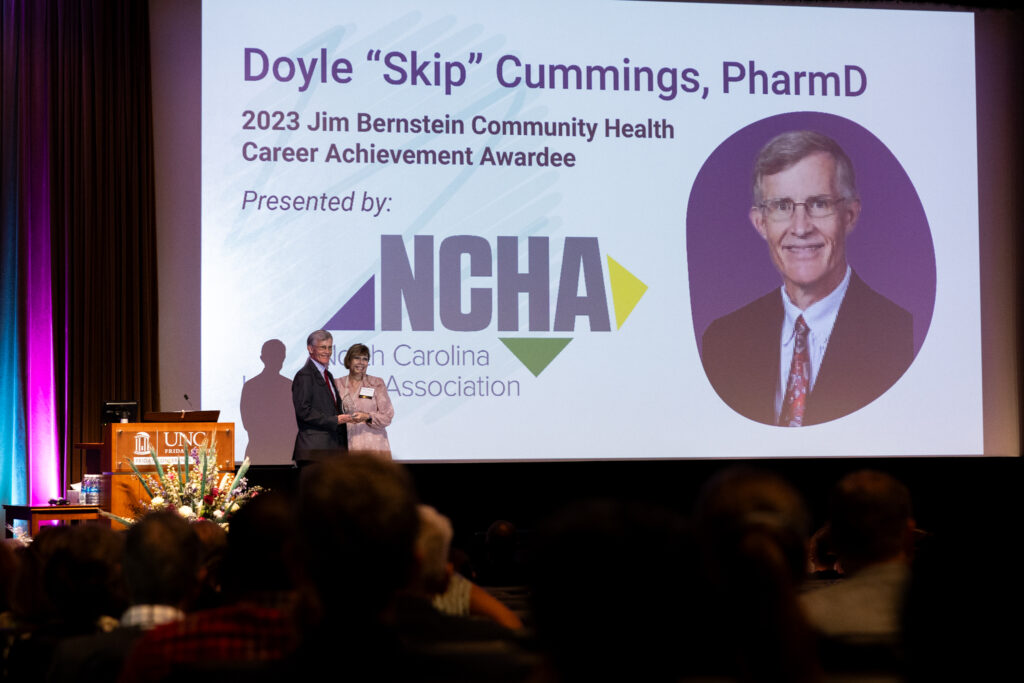
Thank you to all who joined us for this year’s Bernstein Event, for your generous contributions, and for your continued support of Jim Bernstein’s legacy! This year we recognized Dr. Skip Cummings and the Greensboro Health Disparities Collaborative for exceptional leadership improving access and equity in health care, and we presented our first-ever posthumous award to the late Dr. Jim Jones.
Last year was a big year for North Carolina. After a decade of action and advocacy, as of this past December, Medicaid Expansion is finally in effect. This is no small accomplishment, even though it is just one step on the road toward truly healthy and equitable communities. Looking ahead, this policy victory will continue to play a major role as those of us at FHLI continue to act, change systems, and improve health.
2023 was also a big year for FHLI. As we kick off the new year, we’re reflecting on everything we were able to accomplish alongside partner organizations and communities across our state. Read on for highlights from 2023 and look forward to what we have planned for 2024.